In this blog, we spoke to Dr Roger Prudham, Consultant Gastroenterologist, and Dr Sarah Taylor, GatewayC GP Lead, to answer your FIT questions. These questions were asked during live webinars covering FIT, produced in collaboration with NHS England and the Greater Manchester Cancer Alliance Early Diagnosis Team.
FIT for Clinicians
Watch the clinical FIT webinar on-demand
Clinician Q&A
Q: Do we have to send FIT tests from practice off before a certain time in the morning to get tested on the day?
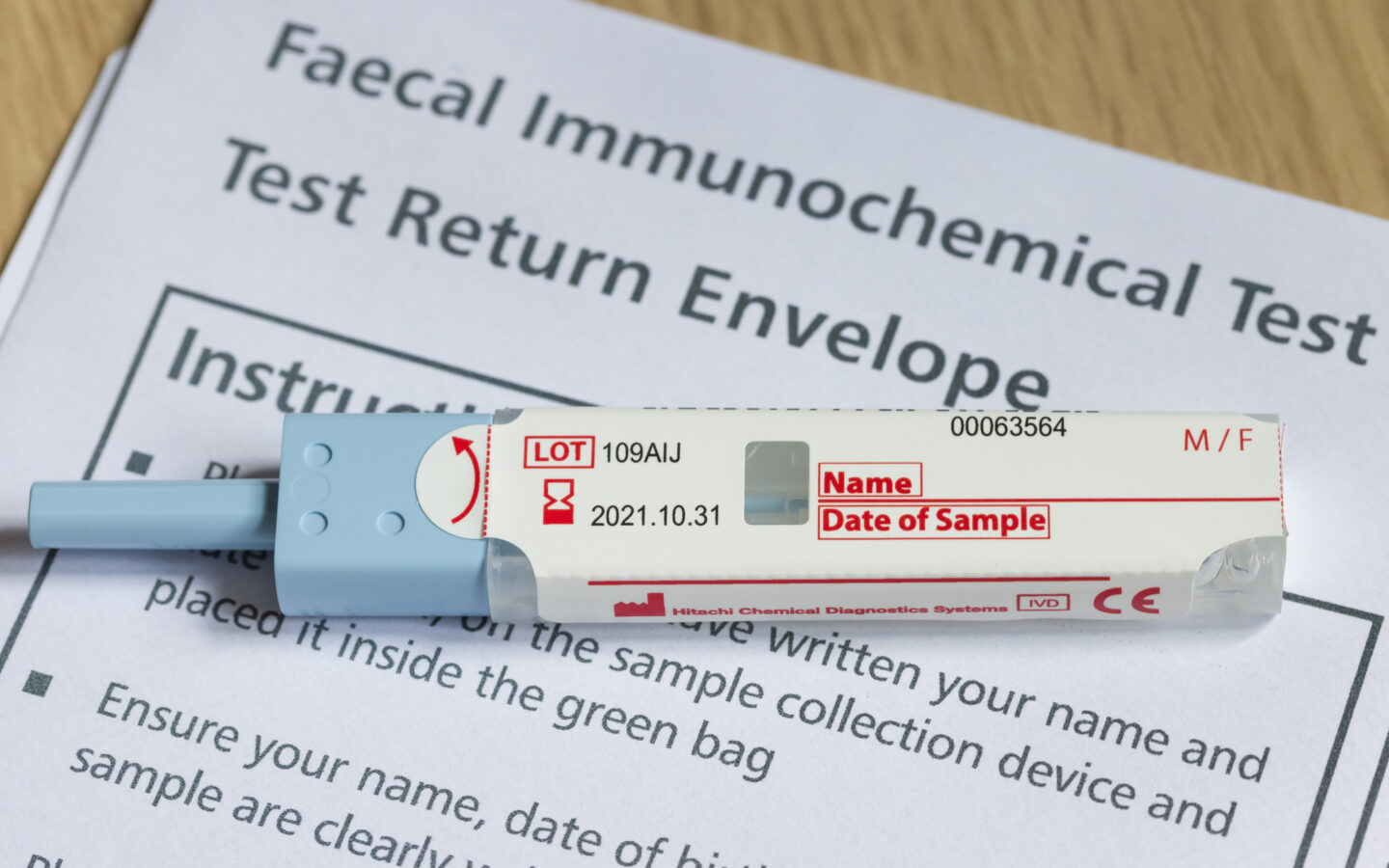
A: FIT can be stored for up to 14 days at ambient temperature after being taken, but this will include the time taken for the patient to send off the sample and transit time. Many trusts will therefore not process a sample that is more than 7 days old. Tests should be sent off ASAP to the lab, and it is important to ensure they are dated.
Q: When talking about a screening FIT, is this referring to the national testing done via the post for eligible groups, as opposed to the tests we request in GP?
A: Yes, that’s correct.
Q: What safety netting do you have in place in your area that helps to get this pathway going?
A: (Dr Sarah Taylor) My practice uses a safety netting template which codes requests so admin staff can search and monitor results.
Q: If a patient has an iron deficiency anaemia and is otherwise asymptomatic with a negative FIT, what would you suggest primary care clinicians do?
A: Watch Dr Prudham, Consultant Gastroenterologist, answer this question.
Q: As the form has only 3 criteria, how do we refer with a negative FIT if we remain concerned about a possible colorectal cancer?
A: Consider referring as a 2WW if you’re concerned and the FIT was negative. Explain your reasons for referral clearly on the form.
Q: If a patient is symptomatic and has a raised FIT but negative lower GI investigations, what’s next?
A: Watch Dr Prudham, Consultant Gastroenterologist, answer this question.
Q: Are FIT requests made via ICE or TQuest coded in the notes?
A: Requests in ICE and Tquest are not coded, you have to take alternative action to code requests.
Q: Are FIT exclusion codes included in the IIF data that is reported on, and therefore those patients are exempt from the set and not included in the percentage of patients being referred in on a LGI suspected cancer pathway?
A: Yes, the patients who have a FIT exclusion code in their record will be excluded from the denominator of LGI referrals in the IIF data for CAN-02.
For reference, the FIT exclusion codes are below and cover the symptoms of rectal/anal mass or anal ulceration. A patient does not need a FIT in primary care and should be directly referred onto the LGI Pathway if they have any of the following symptoms:
| Term | Concept ID | Description ID |
| O/E – PR – rectal mass | 163326007 | 254477013 |
| Ulcer of anus | 20928004 | 35185012 |
| Stercoral anal ulcer | 91105001 | 1235628015 |
| Solitary ulcer of anus | 20928004 | 35186013 |
| Anal ulcer | 20928004 | 35187016 |
| Stercoral ulcer of anus | 91105001 | 150959015 |
| Neoplasm of anal canal | 126850006 | 138013 |
| Tumour of anal canal | 126850006 | 1215967017 |
| Tumor of anal canal | 126850006 | 1217470011 |
| On examination – per rectum – rectal mass | 163326007 | 2668513012 |
| Rectal mass | 248523006 | 370977010 |
| Rectal lump | 248523006 | 370978017 |
For more info, this document covers IIF guidance for 2023/24, including the “Personalised Care Adjustment” which explains the exclusion codes remove patients from the data: Report template – NHSI website (england.nhs.uk)
FIT for Administrators
Watch the administrator FIT webinar on-demand
Administrator Q&A
Q: How long can FIT be stored?
A: Tests can be stored for up to 14 days after taking, but this will include the time taken for the patient to send off the sample and transit time. Many trusts will therefore not process a sample that is more than 7 days old. Tests should be sent off ASAP to the lab, and it is important to ensure they are dated.
Q: Does the position of the sticker on the sample tube matter?
A: Its better if the position of any label that is affixed to the FIT tube is on the opposite edge of the tube to the barcode that comes affixed to the tube.
Q: Are there any other labelling requirements e.g. is the date of the test vital?
A: Specimen labelling requirements for FIT are no different to any other test. A minimum of full name and DOB is essential to avoid rejection. The date of the sample is also helpful. These are the 3 fields on the label supplied on the tube, but most GPs will affix a t-quest label, which is best.
Q: Where do we find translated information for patients?
A: FIT test instructions are available in multiple languages here: https://www.gov.uk/government/publications/bowel-cancer-screening-kit-how-to-use